When did the term hack get substituted for coping strategy? This is an unimportant question that jumped into my head watching the morning newsy show. The gentleman was talking about traveling and airfare and airline scheduling nuances to guarantee getting there on time and not have any trouble. He shared his ideas for traveling early on Thanksgiving day and traveling home Friday. Getting back in time to watch football for the rest of the weekend. He could have FaceTimed his family that he did not want to visit for long. It could have saved a lot of time and money. (That is a hack.)
Wouldn’t it be great to make a list of hacks for Parkinson and his damned disease? He found it. Why did he not write a manual? Even written in the flowery English of the 1800’s it may be of use today. Nevertheless if he published other than his observances to the medical community (The Shaking Palsy – An Essay), I missed it. Parkinson describes a shaking motion. Today his name is associated with a wide range of symptoms, behaviors both movement and cognitive.
In our support group meeting on of the topics posed was “Share one piece of information, a coping strategy (hack), a motivational thought you wish someone had shared with you when Parkinson disease first made an appearance.” I have several and it has taken me a long time to learn them.
Cognitive
Often but not always a person dealing with Parkinson will have cognitive issues in addition to movement issues. These can come in many forms; hallucinations, sensing others, detecting others presence, odd beliefs with little knowledge, delusions, lack of time sense, lack of calendar sense (day), short term memory loss, aphasia, to describe a few. When you detect this happening in the person whom you are helping – Don’t argue. It is very easy to fall into the trap of trying to correct things. Remember with memory loss everyday is a new day.
For me this is an ongoing learning experience. I do use argument (not quite the right term – dissension? – justification?) as a method of attaining her focus because when she is mad at me she is completely focused on what I am saying to her. Often that is when I am attempting to prevent a fall or a near fall. She wants to continue doing something that is to my mind unsatisfactory, bordering on dangerous with her worsening movement control.
I do not do this often because the side effect of having her angry with me can last until bedtime. Sleep I have found is refreshing to her in a way unlike nothing else.
Meds
As a care partner it is extremely important to control meds, medication timing and to observe any issues or effects of the meds. Is this new behavior due to her worsening Parkinson or due to the new med or aging in the old med? It involves lots of reading and observation.
Whenever a change is ordered or a new med is added, the care partner must become observer and research assistant.
Checking activities
Check, check, check on things. A task that might take ten minutes for a non-Parkinson could easily take three times as long. Allow for that when planning activities no matter how small or how large. Parkinson time is different that regular clock time. Many diversions can creep in. In fact scope creep has to be tamped down continuously. (A trip to the toilet can easily morph into putting on a whole new outfit.)
Providing Help
Interfere and help. She may not want your help. Help anyway. Apologize later for helping. Do not help before it becomes apparent that she is truly and hopelessly stuck. Mentally she might think that there is hope yet and she does not need your help. It is also possible that she will not remember you helped. Just help.
Social
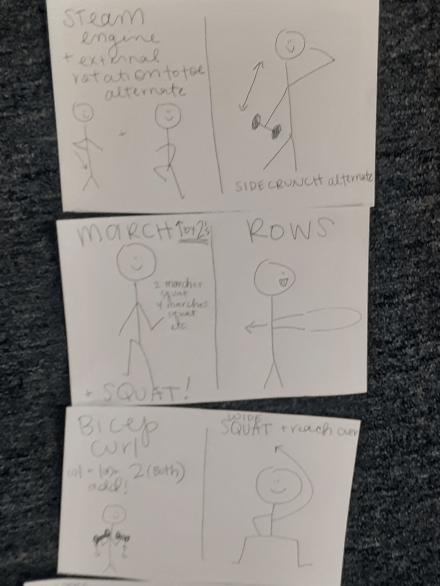
Generate social activities for yourself and your partner. Go out to lunch. Go out to dinner. Visit friends and family. Take walks in the park. As much as your are able look for or create on your own opportunities to be outside and exercise. Seek out exercise venues that cater to people with movement issues. (Physical therapy is one to one. There is very little social interaction.) Specialized exercise classes are far more social.
Socializing in general stretches the brain and often requires dual activity such as eating and talking. Walking and talking in a park is an excellent form of this socialization and has a third benefit of giving the body a chance to make vitamin D. Multitasking is hard for the Parkinson brain.
Caring
You have to create a network of care. You may think you can do it alone. You cannot.
Attitude
Don’t give up. Choose to be happy. And seize the moment.
Don’t be shy – lower your expectations of people
Ask for direct help. Rarely do people when asked for help say no. Usually they say that they cannot right now. Follow up and ask when they can. This can be difficult.
Carpe Diem.